In the United States, over 1.6 million people live without lower limb extremities. Amputations significantly impact the way amputees live, from adjusting everyday activities such as walking to facing the psychological pain of losing a limb.
One of the most common treatments for amputations is a prosthetic, which is an artificial replacement part for the body. While a standard prosthetic can allow for increased movement and independence, it can cause patients pain, discomfort, and soft tissue damage (as prosthetic limbs rely on soft tissue to play the role of a bone). Additionally, these prosthetics make it very difficult for amputees to restore awareness of where that limb should be in space. The amputation and prosthetic process destroy muscles, making it difficult for amputees to control their prosthetics. However, a new form of prosthetic limb brings muscles, bones, and nerves together to reduce these side effects and allow amputees to have more control over a prosthetic limb.
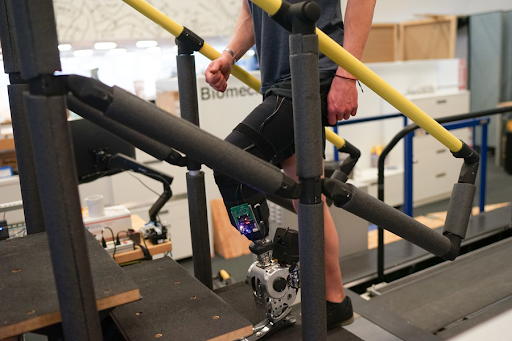
Scientists are trying to create a more user-friendly prosthetic through agonist-antagonist myoneural interface (AMI). According to Science News, “Brain-controlled bionic limbs are inching closer to reality.” Scientists are attempting to unite amputee’s brains with the mechanics of a prosthetic by creating synthetic push-pull pairs, pairs of muscles where one muscle contracts and one muscle relaxes. AMI reconstructs push-pull pairs so amputees can control their prosthetic limb. According to MIT, “A prosthesis driven by the nervous system helps people with amputation walk naturally.” After receiving this new prosthetic, amputees now can walk faster and more naturally than with the standard prosthetic.
Scientists have been researching how to transfer nerve impulses from the brain to prosthetics in order to establish a connection between the nervous system and the prosthetic. In a newly amputated limb, the nerves that once controlled the now nonexistent limb end in empty space, which often causes pain in the area of the amputation. A new technology called targeted muscle reinnervation (TMR) attempts to solve this problem. By stripping muscles of weak nerves and replacing these nerves with stronger nerves, TMR amplifies nervous signals and reduces pain. Through TMR, amputees will be able to control their prosthetic limbs more effectively.
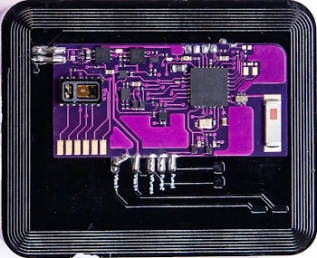
Despite the achievements of TMR, there are only so many muscles in the human body that can be “cannibalized” in this way before space runs out. RPNI, or regenerative peripheral nerve interface, approaches this concept in a different way to try and solve this problem. RPNI places small muscle grafts in the skin and reroutes nerves to these small muscle grafts. For this technique to work, implanted electrodes are used to produce higher-quality nerve signals. While RPNI introduces a solution to the challenges of TMR, it is much more invasive. Researchers at MIT have suggested another approach: osseointegration. Osseointegration uses a titanium bolt to connect the implanted electrodes to the prosthetic and transfer electrical impulses. Osseointegration smoothly connects a person to their artificial limb.
Scientists have already discovered many ways to reduce the pain, discomfort, and tissue damage caused by standard prosthetics. Although this advanced prosthetic still needs to be refined, connecting prosthetic limbs to the brain will have profound impacts for amputees around the world. What began as a prototype in a science lab is becoming reality, with the potential to change lives forever.